Health
HIV AIDS: Where government has gone wrong, What government can do
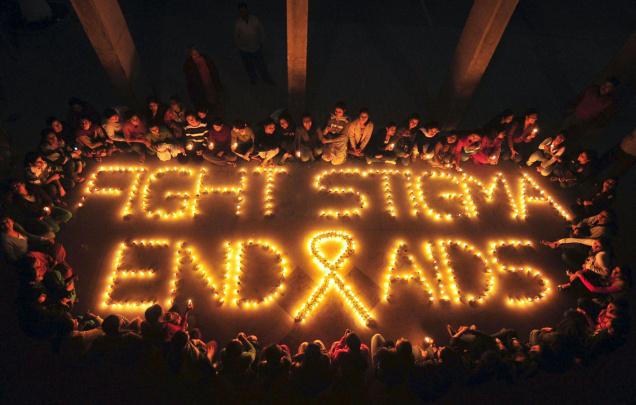
Photo: The Hindu
As another world AIDS day passes by and the epidemic shows no sign of end, we need to evaluate the status of AIDS in India. Our country is one of the hotspot of acquired immunodeficiency syndrome (AIDS), an incurable syndrome that eventually befalls on large fraction of human immunodeficiency virus (HIV) positive individuals. While globally the number of AIDS patients has started to stabilize but epidemic is nowhere close to being over. This global epidemic has already turned out to be a major killer of humankind on an epic scale comparable to black death and smallpox. As per the latest estimates by UNAIDS, it is the fourth leading cause of death. In India, the state of affairs is so unsatisfactory that we still have frequent cases of mass infection of poor patients due to the negligence of hospitals, horrible mistreatment of HIV positive individuals and lack of even basic care for millions of AIDS patients. While the problems of AIDS in India are manifold and would require efforts from all the sectors of Indian society, in this article we want to bring forward key failures of the Indian government. We focus on five core issues that require immediate attention, if we wish to see the tail of this AIDS epidemic:
-
Demographic and epidemiological understanding
-
Awareness
-
Screening and counselling
-
Treatment facilities and medicines
-
Need to develop indigenous cures
Demographic and epidemiological understanding: In India, it is difficult to trust the total number of AIDS patients, as grossly contradicting government figures makes one wonder if the actual magnitude of the epidemic is even larger than what is currently reported. The latest estimates released by the National AIDS Control Organization (NACO), an organization run under the auspices of the ministry of health, indicates that national adult HIV prevalence in India is approximately 0.29%, which corresponds to an estimated 3.4 million plus people living with HIV in our country (Annual report NACO 2009-2010). In contrast in 2005, NACO reported 5.21 millions HIV positive individuals. One can only wonder if such a change in the figures is an effort to put lipstick on the pig or there was a fundamental error in one of the two estimates. There has been some beating around the bush, blame laying and unsatisfactory explanations in response to this contradiction but if there was a genuine error then what is conclusively being done to avoid future errors, is currently not clearly known. Apart from getting the right overall numbers, what is also needed, is detailed demographic and epidemiological data. Different strains of HIV are prevalent in the different parts of the world and progression of AIDS is also different in people of different genetic background, for example there is a very small fraction of people that innately do not contract AIDS. Such trends of immunity to AIDS are either absent or currently not known in the Indian population. It is rather appalling that in India, the land that holds genetic diversity next to the continent of Africa, we for some silly reasons have been using data solely from the White Caucasian populations. This over dependency on western data is wrong for three reasons: 1) The strains of HIV prevalent in different regions are different, 2) The genetic diversity of India makes comparison to one ethnic group meaningless and 3) Apart from the Anglo-Indians with significant European heritage, no ethnic group in India, whatever be their surname and notions of self identity, share that close of genetic identity with the European populations to justify the current usage. What is needed is to understand the spread of different strains of HIV in India and the progression of diseases in individuals with a different genetic background.
Awareness: The first case of AIDS in India was diagnosed way back in 1986. Subsequently some apparent movement of bureaucratic and political machinery took place that in the following year resulted in the formation of National AIDS control program (NACP). In reality, the understanding of Indian government and media on the danger of this disease was largely missing until recently and is still rather poor. Even till late nineties, it was not entirely uncommon to hear voices in the Indian media claiming that AIDS is likely a trouble of promiscuous foreign lands and not of a conservative India. The media and the government forgot that this land of billion plus is first the land of Kamasutra and then of Gandhian moral curtains. Such ethnic biases that come wrapped in moral judgments cost lives everywhere. Even in the United States, initially AIDS was largely thought to be a disease of homosexuals and Afro-Americans, a curse of God for the decadent. In India, the lackadaisical approach in dealing with AIDS was also due to undermining the spread of HIV through blood transfusion and not realizing the severity of needle sharing by drug addicts and poor hospital administrative/clinical measures. As an addition to the existing policy, firstly the government needs to be aware of the full cost of AIDS and then it needs to take action to better inform the health care professionals and public at large. Media also adds to the trouble by rarely looking beyond less glamorous issues than some odd cricketing century of Tendulkar or birth of Bachchan granddaughter, occasionally mentioning somewhat sensational denial of basic services to HIV positive individuals or some innocent people being infected at a mass scale, instead of serious discussion of issues. Serious discussions, even when managing to creep in from the nooks and crannies of the sensational mainstream news, fails to gather attention beyond one media cycle.
Screening and counselling: Roughly 85% of new infections are via the heterosexual route and efforts towards premarital counselling for HIV can reduce half to three fourth of this spread. In Goa and Andhra, the high prevalence states, the state governments proposed bills in 2006 to make HIV testing compulsory before marriage, but ethical concerns and political issues have thus far stopped the actual implementation. This issue of mandatory testing poses a real ethical concern as on one hand we do not have any patient confidentiality where people are denied their due rights due to their HIV status and on the other hand, who can justify the infection to innocent spouses, mostly females via their less than faithful counterparts? One needs to evolve a system where an employer and an insurer, cannot know the HIV status of the patient but a spouse can. It is not going to an easy nut to crack for any government, leave alone Indian, but the administration has not even started inching in the right direction of evolving such a mechanism.
Treatment facilities and medicines: National AIDS control program (NACP-III, 2007-2012) of India has a total budget of about 2.6 billion dollars but only a minor fraction of it is for the treatment. This is unacceptably low amount of money being spent on treatment, especially the amount that finally trickles down the bureaucratic apparatus. One may wonder what do we mean by treatment of an incurable syndrome? The progression of HIV positive individuals to AIDS is very different. Once patient contracts full blown AIDS his/her survival can vary from months to decades. This survival, apart from patient to patient variability, depends on the availability of antiviral drugs and treatment facilities. It is possible that India may have lost much of its potential to produce generic and cheap anti-retroviral relief due to twists in the international politics and India’s easy compliance with pressures. It is possible that recent aid to African countries to counter AIDS, has likely come with strings attached as they have almost stopped use of cheaper generic anti-retroviral drugs. Indian anti-retroviral drugs that were much cheaper than Western products have not just lost a market in Africa but their share in India is also tapering. We would recommend evolution of an informed policy that considers efficacy and costs of all compounds with the goal to save as many lives as possible.
Need to develop indigenous cures: Let us focus on vaccines, a preventative approach that actually holds a long-term cure of AIDS. While there have been some sporadic islands of successes in the ocean of failure in finding vaccine for AIDS, the international efforts are finding new promises and ruling out failed ideas with every passing day. We wonder why not a single significant effort worthy of mention is being pioneered in India? Given that we as Indians have become comfortably numb to the thought of India as a second or third grade country that is a recipient of high-end technology and fruits of scientific research, an average Indian, even if bluntly reminded of the state of affairs, howsoever offended, will not break sweat for long about the lack of innovation. The concern is far graver than the lack of innovation and the lack of national pride. If we need vaccine for AIDS, as soon as it is available in the West, unlike the case with polio or smallpox, we cannot take our begging bowl to world as we did in early years after independence or grossly overpay our way out, as we frequently do to procure any technology, ranging from our medicines to our warplanes. The problem with HIV vaccine stems from to the issues of demographics and epidemiology. Different strains of HIV are prevalent in different parts of the globe. HIV is very diverse, in fact some strains only show 40% homology between each other, not that different of genetic homology between you and a banana and in fact less than you and an earthworm. Thus to combat a hyper-mutable virus one needs to work on local strain and keep local population genetic profile and overall epidemiology in mind to solve the AIDS epidemic in India.
Will India rise to the challenge novel anti-retrovirals and indigenous vaccine? Likely not. Even in the well developed sectors like information technology, India only delivers small software packages for foreign products and does not manufacture a single major internationally recognizable product. This is not due to dearth of scientists or of money. In fact, India has very high numbers of biomedical scientists and research institutions spread across the country for the size of its economy. The problem is of incompetence, lack of management, corruption and nepotism. The political infestation of research is palpable in Delhi where corruption and lack of accountability permeates all levels of research epithet. One need not go into the obvious appointment of unqualified vice chancellors and administrators of universities and directors of research institutes based on proximity to political parties in power. A look at say, the University of Delhi University, a supposed prime University of India, can give you an idea of the political stooges running the show of research in India. Apart from corrupt management, there exist a large number of the so-called scientists who do not have a single major internationally known finding to their name but are busy sliding papers in “friendly” obscure journals and frequently get awarded national and regional honours. This abysmal state of affairs keeps very successful and patriotic scientists out of this Indian swamp that is sure to kill any good science.
In summary, current government efforts are either missing or misplaced and are largely wrought with corruption and inefficiency. A significant blow can be landed to AIDS epidemic with effective government policies. We hope that this article along with many other efforts raises awareness of public and its representatives for better combating the scourge of AIDS.
Health
Experience in clinical quality: What is it, and why is it important?

Ensuring that clinical services are of high quality and adequately meet the needs of patients is essential for any healthcare center. Therefore, they should explore all possible means to achieve these goals. Fortunately, there are specialized consulting firms that offer their knowledge and expertise to help improve the care and services provided.
Experience in clinical quality focuses on the satisfaction patients have with the care they receive at respective healthcare centers. This is crucial because it can impact the patient’s well-being, and therefore, efforts should always be made to enhance it.
What is clinical quality experience?
For a clinic or healthcare center to offer truly high-quality service, it must meet certain parameters that help patients improve their respective health conditions and feel better. Clinical quality expertise refers precisely to the quality of medical care that the patient receives, including their satisfaction and the effectiveness of the services they received. It also relates to the relationship between the patient and the healthcare provider.
This is particularly important because it can affect the health of those receiving treatments and health services. Therefore, clinics and healthcare service providers must strive to improve the patient experience as much as they can, as their patients’ health depends on it.
Fortunately, consulting agencies have specialized in this area and offer advisory services to medical practices, clinics, hospitals, and other healthcare facilities to enhance their services and optimize the clinical quality experience they provide to their patients.
How to improve the clinical quality experience?
There are several ways to improve the clinical quality experience. Firstly, it is essential for healthcare providers to listen to patients and respond to their needs. They should also be kind and compassionate and provide high-quality and effective healthcare.
Similarly, it is important for patients to actively participate in their healthcare, asking questions and expressing their concerns. They should also strictly follow the doctor’s recommendations to improve their health.
Consulting firms are crucial in achieving these objectives as they provide the necessary tools, such as cloud consultations for patients, good practices in pharmacovigilance, development of standardized operating procedures, training, and preparation for health authority inspections. They also analyze possible deficiencies, support data protection, review audit reports and corrective action plans, contributing to the improvement of healthcare processes that all healthcare centers must perform.
Why is clinical quality experience important?
Clinical quality experience is important because it can influence the health and well-being of the patient. If the patient is not satisfied with the medical care received, they are less likely to follow the doctor’s recommendations, which can lead to worsening health problems and dangerous outcomes down the line. Moreover, they are less likely to return to the doctor in the future, putting their health at risk by not having it regularly monitored.
It is essential for the clinic to have a patient experience process that develops appropriate strategies continuously and not just as an isolated action. Every healthcare center should understand the clinical, quality of life, and economic value that such strategies can contribute, recognizing that the patient experience is an ongoing interaction that involves improving communication with the patient in all aspects.
In summary, improving clinical quality experience necessitates strategies like cloud consultations, pharmacovigilance practices, and standardized operating procedures. Consulting firms contribute by analyzing deficiencies, supporting data protection, and refining healthcare processes. The significance of clinical quality experience lies in its influence on patient health, adherence to recommendations, and regular medical monitoring. Continuous improvement in patient experience ensures satisfaction, confidence in physicians, and overall health enhancement. Every healthcare center must recognize the ongoing nature of patient interaction and strategize accordingly for optimal clinical quality experience.
The clinical quality experience should always be optimized so that the patient feels satisfied with the treatments received and has confidence in their treating physicians. This way, they can better evolve their health and prevent any future ailments.
Health
The technological advances in physical and occupational physiotherapy that you should know about

Technology has reached all areas of human life to help us carry out various tasks and to make everyone’s lives easier in different ways. These advances are also in medicine and in the different therapeutic treatments that are used to improve various ailments. Learn what the most advanced methods are and how you can use them.
Health is the most precious thing for every person; extreme care must be taken to ensure the correct functioning of the body. There are many ways and procedures aimed at treating various conditions and helping to stay healthy, which have been significantly enhanced thanks to advances in technology.
The area of physiotherapy is one of those that has taken the best advantage of technological advances, and it has raised the quality and effectiveness of its therapies and procedures to levels never before experienced. Thanks to them, physical and occupational physiotherapy has improved substantially and is increasingly valued for the treatment of various health cases.
Physiotherapy programs for physical rehabilitation
Currently, there are various physical therapy software programs that help patients recover and improve their physical functionality quite efficiently. There is advanced software, with a wide range of physical exercises based on virtual reality, which are designed to promote the progressive and effective recovery of those who find themselves in the need to use them.
Digital physical rehabilitation software includes analytical and functional exercises, which can be used in the rehabilitation of neurological patients, in the recovery of musculoskeletal injuries, in the prevention of falls, in programs against premature ageing and even with children that suffer these types of ailments.
Advantages of using software in physiotherapy
Physiotherapy computer programs are health products, specially designed by professionals, specifically for clinical use. They offer many advantages, among which the following stand out:
- Enjoy the therapy sessions: the gamification that can be achieved with new technologies applied to physiotherapy turns the sessions into truly fun moments, which increases the patient’s motivation and their active participation in performing the corresponding exercises.
- Rehabilitation quantification: all kinematic parameters, such as joint ranges, measurement of the base of support, centre of gravity, number, and characteristics of steps, among others, can be consulted in detail at any time during the therapy. Additionally, they can generate detailed clinical reports on each patient, which can be printed or exported in PDF format.
- Remote sessions: technological advances have reached such high levels that they now open the possibility of applying remote sessions to the patient, thanks to the corresponding home exercise program software for physical therapy designed for this purpose. In this way, treatment can be reinforced with home sessions, which are also monitored and allow remote management, even from the centre itself. This has greatly benefited patients that have mobility problems.
Physical therapy home exercise programs are digital tools that help therapists and patients develop personalised exercise plans from the comfort of their homes. They provide a wide variety of benefits and features that improve rehabilitation and accelerate recovery.
Physiotherapists can decide with which patients and how to develop the digital physical rehabilitation exercises available to them, which can be personalised and adapted according to the needs of each patient.
Occupational therapy software programs
The occupational therapy software programs offer a multitude of resources and tools for therapists and patients, including simulations of everyday tasks, virtual activities to improve fine motor skills, time management strategies, and hand-eye coordination exercises, among others.
One of the main resources used is related to immersive virtual rehabilitation, which allows training various functions of the hand and different movements of the upper extremities that workers perform in their corresponding tasks. To do this, virtual reality and specialised programs are used that simulate environments similar to those they face on a daily basis in their jobs.
These occupational therapy software programs also include patient progress monitoring and assessment tools. They are digital solutions that improve the efficiency of occupational therapy by providing interactive virtual environments and resources tailored to the individual needs of each patient.
Personalization of rehabilitation programs
An important advantage offered by technological advances in this area is the possibility of having personalized rehabilitation programs, which therapists can use to adapt treatments to each patient’s purposes and abilities.
The personalization of rehabilitation programs substantially improves the effectiveness of treatments by addressing the unique needs of each patient. Additionally, this rehabilitation software provides useful resources to monitor and adjust as patients progress in their recovery.
This capacity for adaptation and personalization favours a firmer rehabilitation and speeds up the return to normal functionality of the treated people.
It is a feature that offers various benefits, such as the possibility of applying more individualised approaches, which guarantees that the exercises are safe, effective, and appropriate to promote recovery, and the optimization of results, as they are exercises designed specifically to meet each patient’s needs. .
They also generate greater motivation and adherence, by considering the interests, preferences, and goals of each individual treated, and help prevent additional injuries, since the exercises are adapted to the individual capabilities and limitations of each person.
In conclusion, physical and occupational therapy software has transformed the way rehabilitation is performed on people today. They are digital tools with a wide variety of features that improve the efficiency and personalization of treatments, tailoring the perfect exercise routine for each patient’s needs.
They cover various areas, from home exercise programs to creating personalized exercise plans, facilitating faster and more effective recovery for patients. But, these advances do not stop and aim to continue towards levels that cannot even be imagined, so we can count on an even more promising future in this important area of health.
Do not think about it anymore, if you are suffering from any ailment that could benefit from remote therapy, or know of someone that does, check this software today and see how your life can easily improve thanks to the help of the experts behind them. Your health will thank you.
Health
10 Tips for Starting Your Own Architectural Firm
Are you an architect with a dream of starting your own firm? If so, you’re in luck! Starting your own architectural firm can be a very rewarding experience. However, it’s not without its challenges. This blog post will discuss tips for starting your own architectural firm. With these tips, you’ll be well on your way to launching a successful business!
1) Identify Your Niche:
You’ll need to identify the type of architecture you want to specialize in before getting started. This could be anything from residential homes, commercial buildings, public spaces, or any other niche within the architectural field.
2) Build a Network:
As an architect, your network can make or break your business. Make sure to establish relationships with clients and potential partners as soon as you can. Joining local networking groups and attending events can help you build valuable connections.
3) Secure Funding:
If you don’t have enough capital to get started, consider applying for grants or loans from government agencies or investors. Having some capital behind you will give you more freedom to pursue projects that align with your goals and vision for your firm.
4) Develop a Business Plan
A successful business requires a plan. Your plan should include your vision for the firm, as well as strategies for marketing and managing finances. Having a clear roadmap to follow will make it easier to stay on track and reach your goals.
5) Protect Yourself Legally
It’s important to protect yourself legally when starting an architectural firm. Make sure you understand all of the relevant laws in your area, including licensing requirements and zoning regulations. You’ll also need liability insurance in case something goes wrong with one of your projects.
6) Invest in Technology
In order to keep up with the competition, you’ll need to invest in modern technology and tools. This could include anything from computer-aided design (CAD) software to a paper folding machine. Investing in the right technology can help you streamline processes, save time, and create a better final product.
7) Marketing
Marketing is key to the success of any business. Make sure you have a good plan in place for reaching out to potential clients and increasing your visibility. Social media, content marketing, and search engine optimization (SEO) can all be helpful in this regard.
8) Hire Talented Employees
If you want your firm to stand out from the competition, you’ll need to hire talented employees. Look for individuals with experience in the architectural field who share your vision and passion for design.
9) Develop a Brand
Creating a unique brand identity is essential if you want your firm to stand out from the crowd. This could involve creating a logo, website, or slogan that captures the essence of what your firm stands for.
10) Stay Flexible
The architecture industry is constantly changing and evolving, so it’s important to stay flexible and adapt to new trends. Don’t be afraid to try something different or take risks when necessary. Doing so can lead to greater success in the long run.
Starting your own architectural firm can be a rewarding experience, but it requires planning and dedication. Make sure to follow these tips when getting started to ensure that you set yourself up for success!
-

 Business9 months ago
Business9 months agoHow To Future-Proof Your Business With The Right Tools
-

 Travel7 months ago
Travel7 months agoTravelling from San Antonio to Guadalajara
-

 Business11 months ago
Business11 months agoThe importance of telescopic handlers: innovation and efficiency in load handling
-
 Travel12 months ago
Travel12 months agoDiscover extraordinary places and enjoy unique experiences
-

 Business10 months ago
Business10 months agoWhat are EDC products, and why should you always have them?
-

 Travel4 months ago
Travel4 months agoTravel wellness tips for a healthier and more enjoyable journey
-

 Europe2 months ago
Europe2 months agoRecent Books by Boaventura de Sousa Santos: Law, Colonialism, and the Future of Europe







